Utility of intraoperative electrophysiology in intrathoracic resection of schwannoma
Sancho-Hernández, Rogelio1; Marhx-Bracho, Alfonso1; Solorio-Rodríguez, Lizbeth1; Mata-Favela, Nadia Nohemí1
Sancho-Hernández, Rogelio1; Marhx-Bracho, Alfonso1; Solorio-Rodríguez, Lizbeth1; Mata-Favela, Nadia Nohemí1
ABSTRACT
KEYWORDS
schwannoma, brachial plexopathy, case report, neurophysiological monitoring.Introduction
Primary tumors of the brachial plexus are infrequent entities and correspond to schwannomas and neurofibromas, these are approached as cervicomediastinal masses with apical intrathoracic extension, and may debut with symptoms of vascular and neural compression.1
The clinical presentation of an adolescent girl with brachial plexus schwannoma is described with the technical-surgical details of its resection assisted by neurophysiological evaluation. There are no national reports of this novel intervention in the pediatric population.
Case presentation
14-year-old female diagnosed with neurofibromatosis type I, since the age of 10 years with ascending pain throughout the left upper limb to the neck, with paresis and paresthesia, atrophy and decreased muscle strength, weight loss of 7 kg; with generalized "coffee with milk" dermatosis, enlargement with left hemicollar base, painful, asymmetry of the left thoracic limb at the expense of atrophy of interosseous, tenar and hypothenar muscles, functional limitation, generalized hyperreflexia, preserved proprioceptive and exteroceptive sensitivity.
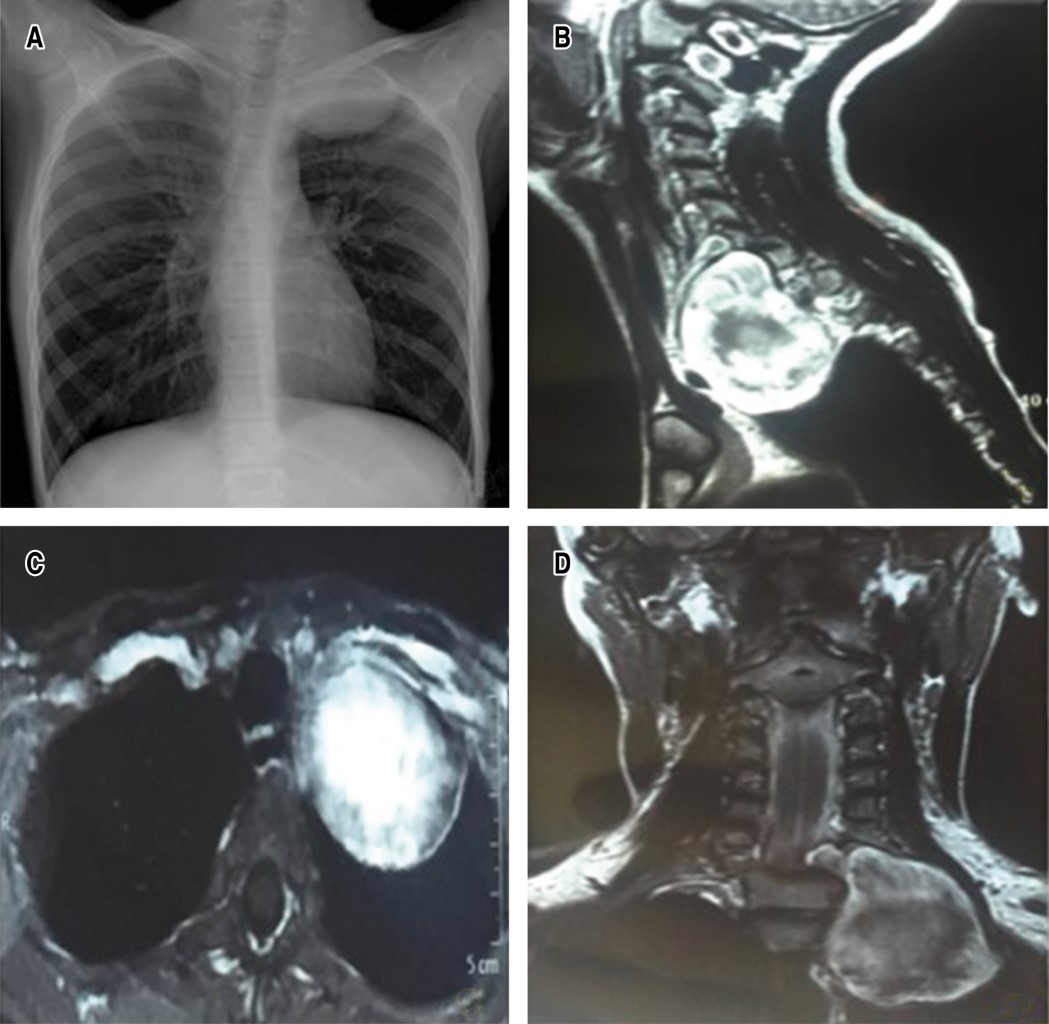
Magnetic resonance imaging shows extradural lesion originating at the level of the left C7-T1 conjunctival foramen, widening and rostral extension towards the neck and displacement of the trachea and esophagus and in contact with the carotid sheath and invasion towards the ipsilateral mediastinal region. Electromyography was performed, showing a decrease in the amplitude of sensory and motor latencies of the left ulnar nerve (Figure 1A-D).
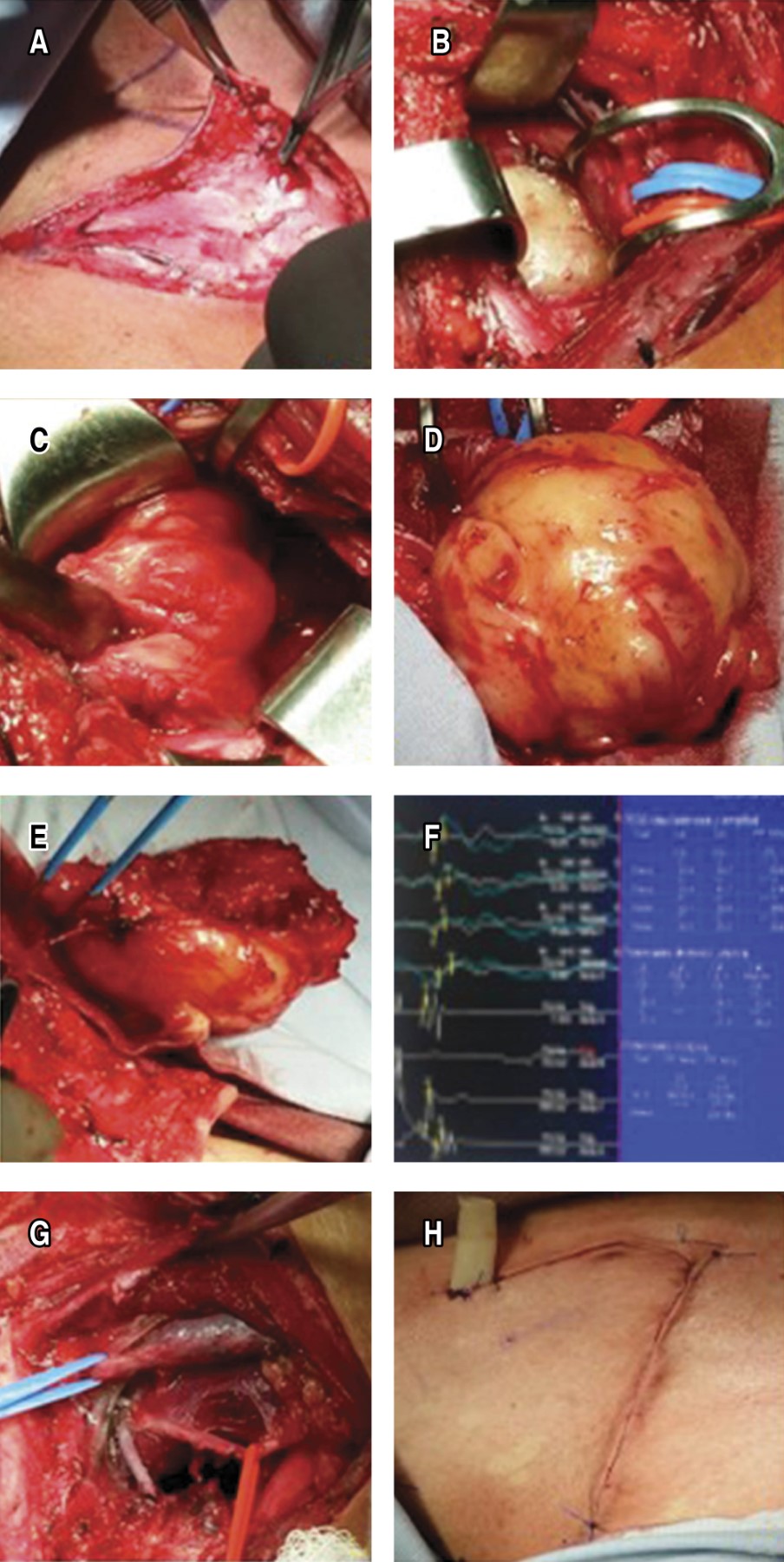
Tumor excision was performed through anterior cervicothoracic approach with neurophysiological monitoring, finding: spherical mass of 9 × 7 × 5 cm and encapsulated, resected by central and intracapsular enucleation dependent on C5, C6 and C7 nerve roots, extrapleural corroborated by a left thoracoscopic approach, without drains.
The pathology report is a diagnosis of cervicothoracic schwannoma. At two weeks' post-surgery, the patient had recovered mobility but continued with significant atrophy; however, he presented gradual recovery of muscle tone and strength and movement in the affected limb at seven years of follow-up with rehabilitation support (Figure 2A-H).
Discussion
Schwannomas are usually benign extrathoracic and supraclavicular masses, intrathoracic and mediastinal growth are rare and, even more so, in the pediatric population, with few reports in the literature; but they are the most common intrathoracic neurogenic tumors.2,3 In our case, this encapsulated and peripheral tumor contrary to neurofibromas originated from the nerve sheath around the brachial plexus receiving irrigation from the axillary subclavian trunk. They may present with symptoms of nerve compression with neurological deficit, distal pain, sensory loss and weakness, with a palpable cervicothoracic mass being the most common initial presentation.4
Color Doppler ultrasonography and tomography could show that the nerves enter eccentrically to the schwannoma, which in turn is not observed in neurofibroma (main differential diagnosis and prognosis); however, schwannomas are iso to hypointense in T1 and hyperintense in T2 of gadolinium magnetic resonance imaging, defining the preoperative anatomical relationships as a study protocol of the brachial plexus and thoracic sulcus.5,6 However, the hard and invasive consistency of the lesion associated with systemic symptoms with adenopathies could propose fine needle aspiration biopsy as an alternative to predict a final diagnosis. In our case, the diagnostic association with neurofibromatosis type I was suggestive of brachial plexopathy due to schwannoma.2
The use of S100 protein in the pathologic diagnosis of neural crest tumors is very popularized and associated with microscopic findings of spindle cells with areas of myxoid stroma with striated bundles of dense collagen, as occurred in our report. SOX10 protein is a more sensitive and specific marker than S100 for schwannoma and melanocytic tumors, especially in those diagnostic situations where sarcoma-like morphologic changes can be demonstrated. Calretinin is detected in almost all schwannomas and only in a small percentage of neurofibromas, which adds an important differential diagnostic marker.2
Surgery is indicated for tumors that cause neurological deficits, progressive lesions with suspected malignancy and to prevent or minimize neural damage, with complete surgical excision by enucleation of the schwannoma and dissection and preservation of the nerve fascicles being the most recommended surgical approach.4,7 In our case, an anterior supraclavicular cervicothoracic approach combined with a left thoracoscopic approach was initially considered to safely manipulate the vascular and nerve structures of the thoracic outlet and to rule out potential intrapleural involvement of the lesion. However, series have found that a neurological deficit of 5% preoperatively increases to 11.5% after resection of schwannoma and brachial plexus neurofibromas, so nerve sparing as possible is important to maintain the patient's motor function.3,4
The causes of postoperative neurological deficits are related to preoperative nerve compression, mechanical injury or transoperative ischemia, reoperations associated with incomplete enucleation. Therefore, several perioperative neurological monitoring methods have been developed, such as spontaneous electromyography (EMG), somatosensory evoked potentials (SEP) and nerve action potentials (NAP).8 With EMG, nerve stimulation is performed and muscle activity is recorded to identify or avoid nerve damage; with SEP, it is useful for recording brachial plexus lesions and evaluates whether there is continuity with the central nervous system; with NAP, the nerve trunk proximal to the lesion area is directly stimulated and a recording is obtained in the area distal to the lesion; it is useful in nerve lesions due to continuity and determines the need for other reconstruction procedures with sural nerve grafts. The critical steps in surgical resection of brachial plexus schwannoma with electrophysiological monitoring in our case were: a) exposure of the nerve proximal and distal to the tumor by neurolysis; b) capsular exposure and electrostimulation of the tumor to localize and map the functional nerve distribution; c) longitudinal incision of the capsule in the direction of adjacent nerves with no recordable functional activity; d) enucleation and electrostimulation to avoid damage to functional nerve fibers; e) final exposure of the proximal and distal poles of the tumor where the nerves run and evaluation by NAP to determine a potential continuity injury requiring reconstruction with sural graft; and f) postoperative monitoring of basal and functional deficits for future rehabilitation and prognosis.
The schwannoma, in our case, facilitated surgical separation of healthy and functional nerve fibers; neurorrhaphy or sural grafting was not necessary as described for neurofibromas and primary malignancies; the anterior cervicothoracic approach with an L-shaped incision was sufficient. However, the cervico transsternal trap-door approach should be considered for invasive masses with a large intrathoracic and mediastinal component.9,10
Conclusions
The approach to masses located at the cervicothoracic junction represents a surgical challenge, both because of their location in contact with vascular and nervous structures, and because of the adequate control and management that must be carried out to avoid complications such as chronic pain and alterations in limb mobility, transoperative neurophysiological monitoring increases safety and perioperative prognostic benefit.
AFILIACIONES
1Instituto Nacional de Pediatría, Mexico City, Mexico.Acknowledgments: Pediatric Intensive Care Unit, National Institute of Pediatrics, Mexico.
Conflict of interests: the authors declare that they have no conflict of interests.
REFERENCES
Siqueira MG, Martins RS, Teixeira MJ. Management of brachial plexus region tumours and tumour-like conditions: relevant diagnostic and surgical features in a consecutive series of eighteen patients. Acta Neurochir (Wien). 2009;151(9):1089-1098. Available in: https://doi.org/10.1007/s00701-009-0380-8