Characterization of malignant endobronchial lesions
Rabadan-Armenta, Saul Javier1; García-Torres, María Elena1; Hernández-Hernández, Mario Abel1
Rabadan-Armenta, Saul Javier1; García-Torres, María Elena1; Hernández-Hernández, Mario Abel1
ABSTRACT
KEYWORDS
bronchoscopy, squamous cell carcinoma of the lung, lung adenocarcinoma, endobronchial tumor, bronchoscopic findings.Introduction
Bronchoscopy is a visualization technique of the upper and lower airways that is used for diagnostic or therapeutic purposes. This technique is useful for diagnosing inflammatory, infectious, tumor and hemorrhagic processes.1
The most common neoplastic lesions in the bronchi are secondary to bronchogenic carcinoma, representing only 1% of extrathoracic tumors.2 The incidence varies according to the literature and depends on the evolutionary stage of the primary disease, the group of patients studied and the follow-up program.3 The reported prevalence of visible endobronchial metastases in the main or lobar bronchi is 2%.4
For the clinical study of these patients, minimally invasive diagnostic methods such as chest radiography and computed tomography (CT) of the chest are commonly initiated. These methods may provide indirect or suggestive data of airway compromise. Bronchoscopy is the chosen study for the identification and evaluation of lesions in the central airway. Based on the radiological findings, it is determined which patients are candidates for fibrobronchoscopy for tissue sampling and subsequent histopathological analysis.
Flexible bronchoscopy is an invasive procedure that allows direct visualization of the airway and sample collection by bronchoalveolar lavage, bronchial brushing or biopsy. At the General Hospital of Mexico, Mexico City, flexible bronchoscopy has a crucial role in the diagnosis of tumors with suspected airway malignancy.
The main objective of this study is the characterization of endobronchial lesions with suspected malignancy and their correlation with histopathologic findings.
Material and methods
Retrospective analysis of cases of patients with suspected malignant lung lesion or lung cancer brought to the Bronchoscopy area of the General Hospital of Mexico from 2018 to 2023. Demographic data, imaging studies, bronchoscopic images and pathology findings were reviewed.
The diagnostic suspicion of lung cancer and pulmonary metastasis was established based on anamnesis, clinical evaluation, and chest X-ray and CT findings. First of all, flexible bronchoscopy was used to obtain the sample, as well as surgical biopsy in patients in whom no diagnosis was obtained by flexible bronchoscopic biopsy and/or no lesion was evident to perform bronchoscopic sampling.
The histological diagnosis was confirmed by biopsy of the identified lesion, in addition to bronchoalveolar brushing and lavage. Endobronchial metastasis was defined as single or multiple lesions visible through bronchoscopy, compromising the trachea, tubes or segmental bronchi, and with histology equal to the primary extrathoracic malignancy.
The main bronchoscopic findings and the number of bronchi affected were correlated with the malignant lesion confirmed by histopathology and the number of metastases in the patient. The presence of mucosal infiltration, endobronchial tumor, hypervascularization, irregular and hypervascularized edematous mucosa were considered as suspicious findings of malignancy. Other variables such as extrinsic compression were also evaluated.
Statistical analysis: was performed using Microsoft Excel and IBM Statistical Package for the Social Sciences (SPSS), version 20.0.
Characteristics of the equipment and procedures applied: the EB-1970K Pentax videobronchoscope, with a 2.8 mm working channel was used. Cook alligator bronchoscopy forceps and a protected brush were used for post-biopsy cytology. In total, 3 to 5 biopsies were performed during bronchoscopies that were conducted with narrow band imaging (NBI).
Results
Demographic characteristics
A total of 122 patients were included, including 52 women (42.6%) and 70 men (57.4%), the mean age was 62 years with values ranging from 46 to 82 years.
Imaging studies
Chest radiography was the initial diagnostic imaging method used, the radiological features found were single parenchymal opacity in 43 (35.2%) patients; multiple parenchymal opacities in 21 (17.2%); pulmonary cavity in nine (7.4%); enlargement of the pulmonary hilum in 17 (13.9%); atelectasis in 12 (9.8%); unilateral pleural effusion in six (4.9%); bilateral pleural effusion in five (4.1%); no alterations were identified in the chest X-ray in nine (7.4%) cases.
Chest CT with contrast was performed on 48 patients before the study with the following findings: 32 (66.7%) patients with tumor lesion; six (12.5%) patients with obstructive pneumonia; 18 (37.5%) with atelectasis; parenchymal tumors were located in the right lung in 28 (58.3%) patients and left lung in 20 (41.7%). Hilar and prebronchial lymphadenopathy was found in 33 patients (68.8%), three with pleural effusion (6.3%).
Bronchoscopic study
Bronchoscopy was performed in all 122 patients due to chest X-ray and/or computed tomography findings. Of these, 100 patients underwent biopsy, brushing and bronchoalveolar lavage for cytological study.
The bronchoscopic features of the lesions observed were as follows (Table 1):
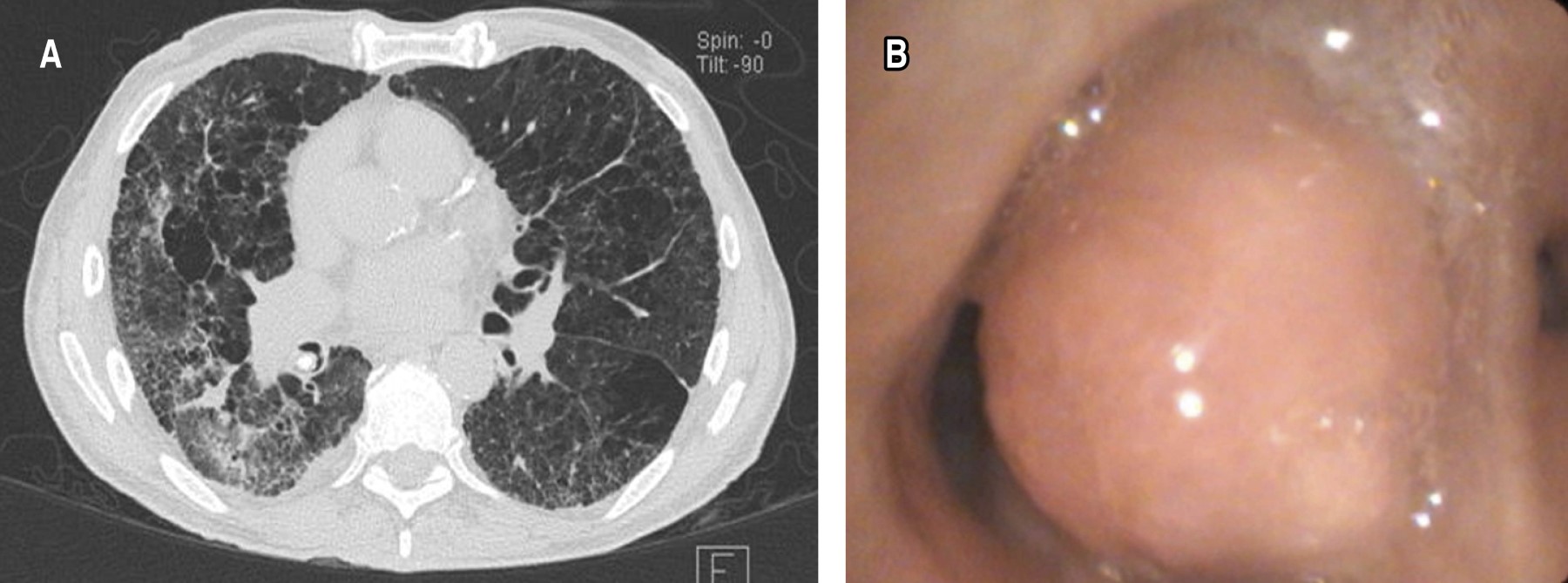
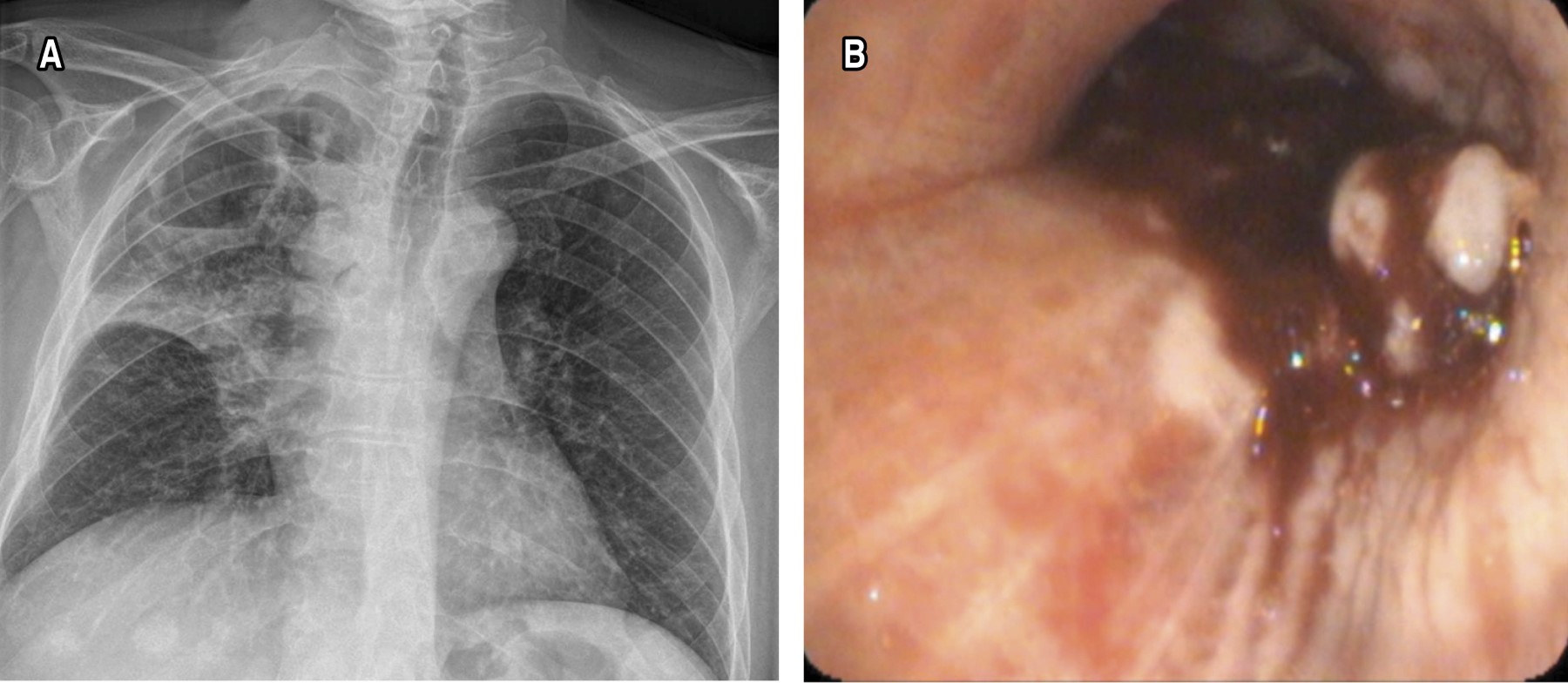
Sixty-four endobronchial tumors were identified, the most frequent location was in the right bronchial tree, with 39 (60.9%) patients. Of these, 19 (29.6%) were found between segments 6 to 10 right, 12 (18.7%) in the middle lobe and eight (12.5%) in segments 1 to 3. In the left bronchial tree, 25 cases (39%) were observed. Of these, six (9.3%) were found between left segments 6 to 10, 10 (15.6%) in the lingula and nine (14%) in segments 1 to 3 (Figures 1 and 2).
Mucosal infiltrative lesions with increased vascularization were observed in 21 patients.
Extrinsic compression of the bronchial wall was identified in 15 patients.
Bronchoscopically normal appearance of the bronchial tree mucosa was found in 14 subjects.
Pale and atrophic mucosa was found in 34 patients.
Erythematous and edematous mucosa was identified in 22 cases.
Abundant bronchial secretions were reported in 15 patients, while moderate bronchial secretions were observed in 22.
Combinations of these lesions were found especially in mucosal characteristics.
Biopsies were taken, as well as brushing and cytological lavage of the following lesions:
Of the 64 endobronchial tumors, biopsies were performed, as well as bronchioloalveolar brushing and lavage.
The histopathological result of the biopsy was positive in 98.4% of the cases (63 patients), brushing showed a diagnosis in 7.8% (five patients) and bronchioloalveolar lavage only reported cells compatible with malignancy in 1.6% (one patient) (Table 2).
Mucosal infiltrative lesions with increased vascularization were observed in 21 patients and biopsies were taken, as well as bronchioloalveolar brushing and lavage.
Histopathological analysis of the biopsy was positive in 81% (17 patients), brushing was diagnostic in 4.8% (one case) and bronchioloalveolar lavage did not report cells compatible with malignancy in any patient.
Finally, extrinsic compression of the bronchial wall was identified in 15 patients and biopsies were obtained, as well as bronchioloalveolar brushing and lavage.
Biopsy was positive in 13.3% (two patients), brushing was not diagnostic in any patient and bronchioloalveolar lavage did not report cells compatible with malignancy in any patient.
Histopathology
The results obtained from the samples collected by bronchoscopy were as follows:
Of the 63 endobronchial tumor samples, 24 (38.1%) corresponded to squamous cell carcinoma, 19 (30.2%) to adenocarcinoma, eight (12.7%) to small cell lung cancer, five (7.9%) to infiltrating ductal carcinoma, four (6.3%) to germinal tumor and three (4.8%) to clear cell renal carcinoma.
As for mucosal infiltrative lesions with increased vascularization, of the 17 patients, 13 (76.5%) corresponded to adenocarcinoma and six (35.3%) to squamous cell carcinoma. Two patients with extrinsic compression presented pulmonary adenocarcinoma.
In total, by histopathology of bronchoscopy samples, 30 (23.8%) cases were diagnosed with squamous cell carcinoma, 34 (27.0%) with pulmonary adenocarcinoma, eight (6.3%) with small cell lung cancer, five (4.0%) with infiltrating ductal carcinoma, four (3.2%) with germinal tumor and three (2.4%) with clear cell renal carcinoma.
Discussion
Lung cancer remains one of the leading causes of death worldwide, with high mortality rates because most cases are diagnosed in advanced stages. Like other malignant neoplasms, lung cancer can present endobronchial metastasis, complicating its diagnosis and treatment even more. In this context, chest X-rays and CT scans are key tools for the initial identification of lung lesions. In our study, chest radiographs revealed pathological features in most patients, with alterations such as parenchymal opacities, hilar enlargement and pleural effusion, which coincided with reports in the literature, where radiography continues to be useful in the initial detection of neoplastic pathologies.5
Contrast-enhanced computed tomography was also crucial in the evaluation of suspicious lung lesions, providing more precise anatomical details. Tumor lesions were identified in 66.7% of patients and hilar and prebronchial lymphadenopathy was observed in 68.8%, which highlights the importance of this technique in the evaluation prior to more invasive procedures such as bronchoscopy.5
As for endobronchial neoplasms, despite their rarity, they represent a considerable diagnostic and therapeutic challenge. In our study, different histological subtypes were documented, with a predominance of squamous cell carcinoma (38.1%) and adenocarcinoma (30.2%). These findings differ from those reported in the literature, where carcinoid tumors and mucoepidermoid carcinoma are usually the most common.1,2 In addition, we identified rare secondary tumors, such as infiltrating ductal carcinoma and clear cell renal carcinoma, highlighting the complexity of endobronchial metastases, the prevalence of which is low but clinically significant.3,4
It is relevant to mention that endobronchial metastases are usually a late sign of the disease, which coincides with what was found in this study, since bronchoscopy allowed the diagnosis of the primary tumor in all cases, but already at an advanced stage. This finding underscores the need for more effective tools for early detection of these lesions.6
Regarding the diagnostic tools available today, it is essential to highlight the importance of advanced technologies in bronchoscopy, such as narrow band imaging (NBI), bronchial autofluorescence (BAF) and high-magnification bronchoscopy. These modalities allow detailed visualization of mucosal and vascular lesions, facilitating the detection of suspicious high-grade lesions. NBI, for example, uses blue and green light to highlight the vascularization and structure of the mucosa, improving the identification of areas of dysplasia and neoplasia at early stages.7,8
Also, newer technologies, such as optical coherence tomography (OCT) and confocal laser endomicroscopy (CLE), are emerging as promising tools in the real-time evaluation of endobronchial lesions. OCT, which provides near-histological images, has proven useful for tumor characterization and assessment of airway remodeling,9 while CLE allows in vivo imaging of the tumor microenvironment in great detail, which could improve early diagnosis of cancers and assessment of response to treatment.10
In our study, bronchoscopy with biopsy was the most effective diagnostic method, with a positive yield in 98.4% of cases, which is in agreement with the literature, where bronchoscopic biopsy is considered the gold standard for the evaluation of intraluminal lesions.11 However, it is important to consider the low sensitivity of other techniques, such as bronchial brushing and bronchioloalveolar lavage, which highlights the need for a combination of diagnostic methods to optimize results.12
In a recent prospective study, brushing performed before biopsy with endobronchial forceps significantly increased diagnostic yield compared to brushing after biopsy. The overall diagnostic yield of brushing for detecting malignancy in visible endobronchial lesions is about 60 to 90%.13 The diagnostic yield of endobronchial biopsy for visible endobronchial tumors is at least 70%.14 Bronchioalveolar lavage (BAL), commonly used as an adjunct to other bronchoscopic sampling modalities for the diagnosis of malignant neoplasms, has a diagnostic yield of less than 50% in most studies, but this percentage is higher than 80% in lymphangitic carcinomatosis.15
Finally, although there are no well-established guidelines for the management of endobronchial tumors, treatment should be individualized, considering the location of the primary tumor, the patient's characteristics and the general state of the disease. Since in many cases these lesions represent a late sign of systemic metastasis, a multidisciplinary approach integrating bronchoscopic findings with other imaging modalities and histological studies is essential to guide therapeutic decisions.11
As for complications associated with transbronchial biopsy (TBLB), the most common include pneumothorax and bleeding.16 The rate of pneumothorax varies between 1 and 5% in the general population, but is higher in the presence of risk factors such as surrounding emphysema or the use of mechanical ventilation.17 However, no cases of pneumothorax were documented in our study, which could be attributed to careful patient selection and the experience of the medical team.
Conclusions
Endobronchial lesions in this study remain a late diagnosed condition. Bronchoscopy is still the most important invasive method of diagnosis. One of the important advantages is that it allows the visualization of lesions, in addition to taking a biopsy. Among the most common lesions are endobronchial tumors and mucosal infiltration. Adenocarcinoma is the most frequent form found in our patients. Bronchoscopy has allowed us to give a correct histopathological diagnosis without the complications of surgical interventions, less severe post-surgical complications and better recovery.
AFILIACIONES
1Hospital General de México, Mexico City, Mexico.Conflict of interests: the authors declare that they have no conflict of interests.
REFERENCES
Wahidi MM, Govert JA, Goudar RK, Gould MK, McCrory DC; American College of Chest Physicians. Evidence for the treatment of patients with pulmonary nodules: when is it lung cancer? ACCP evidence-based clinical practice guidelines (2nd edition). Chest. 2007;132(3 Suppl):94S-107S. Available in: https://doi.org/10.1378/chest.07-1352
|
Table 1: Bronchoscopic findings and correlation with diagnostic methods (N = 122). |
|||
|
Bronchoscopic appearance |
Biopsy n (%) |
Brushing n (%) |
Bronchioloalveolar lavage n (%) |
|
Endobronchial tumor (n = 64) |
63 (98.4) |
5 (7.8) |
1 (1.6) |
|
Mucosal infiltrative lesions with increased vascularization (n = 21) |
17 (81) |
1 (4.8) |
0 (0) |
|
Extrinsic compression of the bronchial wall (n = 15) |
2 (13.3) |
0 (0) |
0 (0) |
|
Table 2: Chest radiographic and computed tomography findings. |
||
|
Radiological finding |
Chest X-ray N = 122 n (%) |
Chest tomography N = 48 n (%) |
|
Single parenchymal opacity |
43 (35.2) |
— |
|
Multiple parenchymal opacities |
21 (17.2) |
— |
|
Lung cavity |
9 (7.4) |
— |
|
Enlargement of the pulmonary hilum |
17 (13.9) |
— |
|
Atelectasia |
12 (9.8) |
18 (37.5) |
|
Unilateral pleural effusion |
6 (4.9) |
3 (6.3) |
|
Bilateral pleural effusion |
5 (4.1) |
— |
|
No alterations |
9 (7.4) |
— |
|
Tumor lesion |
— |
32 (66.7) |
|
Obstructive pneumonia |
— |
6 (12.5) |
|
Hilar and prebronchial lymphadenopathy |
— |
33 (68.8) |